Dr. Dean Dornic
Dr. Dean Dornic
Chosen by His Peers as One of America's Top Ophthalmologists
Dr. Dean Dornic
3701 NW Cary Parkway
Suite 101
Cary, NC 27513
ph: (919) 467-9955
fax: (919) 467-2544
drdeando
 There has been a lot of press regarding the safety and efficacy of LASIK. The following is an abstract from the leading authoratative Journal on eye care: Ophthalmology.
There has been a lot of press regarding the safety and efficacy of LASIK. The following is an abstract from the leading authoratative Journal on eye care: Ophthalmology.
Wavefront-Guided LASIK for the Correction of Primary Myopia and Astigmatism:A Report by the American Academy of Ophthalmology
Steven C. Schallhorn, MD, Ayad A. Farjo, MD, David Huang, MD, PhD, Brian S. Boxer Wachler, MD, William B. Trattler, MD, David J. Tanzer, MD, Parag A. Majmudar, MD, Alan Sugar, MD, MSReceived 28 March 2008; received in revised form 28 March 2008; accepted 8 April 2008.
Objective
To describe wavefront-guided (WFG) LASIK for the primary treatment of low to moderate levels of myopia and astigmatism and to examine the evidence on the safety and effectiveness of the procedure in comparison with conventional LASIK.
Methods
Literature searches conducted in 2004, 2005, 2006, and 2007 retrieved 209 unique references from the PubMed and Cochrane Library databases. The panel selected 65 articles to review, and of these, chose 45 articles that they considered to be of sufficient clinical relevance to submit to the panel methodologist for review. During the review and preparation of this assessment, an additional 2 articles were included. A level I rating was assigned to properly conducted, well-designed, randomized clinical trials; a level II rating was assigned to well-designed cohort and case-controlled studies; and a level III rating was assigned to case series, case reports, and poorly designed prospective and retrospective studies. In addition, studies that were conducted by laser manufacturers before device approval (premarket approval) were reviewed as a separate category of evidence.
Results
The assessment describes studies reporting results of WFG LASIK clinical trials, comparative trials, or both of WFG and conventional LASIK that were rated level II and level III. There were no studies rated as level I evidence. Four premarket approval studies conducted by 4 laser manufacturers were included in the assessment. The assessment did not compare study results or laser platforms because there were many variables, including the amount of follow-up, the use of different microkeratomes, and the level of preoperative myopia and astigmatism.
Conclusions
There is substantial level II and level III evidence that WFG LASIK is safe and effective for the correction of primary myopia or primary myopia and astigmatism and that there is a high level of patient satisfaction. Microkeratome and flap-related complications are not common but can occur with WFG LASIK, just as with conventional LASIK. The WFG procedure seems to have similar or better refractive accuracy and uncorrected visual acuity outcomes compared with conventional LASIK. Likewise, there is evidence of improved contrast sensitivity and fewer visual symptoms, such as glare and halos at night, compared with conventional LASIK. Even though the procedure is designed to measure and treat both lower- and higher-order aberrations (HOAs), the latter are generally increased after WFG LASIK. The reasons for the increase in HOA are likely multifactorial, but the increase typically is less than that induced by conventional LASIK. No long-term assessment of WFG LASIK was possible because of the relatively short follow-up (12 months or fewer) of most of the studies reviewed.
Acuracy of LASIK Improves
Nov. 7, 2008 American Academy of Ophthalmolgy Meeting
ATLANTA — In the literature, 95% of myopic patients are achieving uncorrected visual acuity of 20/20 after custom laser vision correction, a surgeon said here. In custom hyperopic patients, similar success is being reported in 70% to 80% of cases.
"In the old days, 7 years ago, we were seeing maybe 95% 20/40 or better uncorrected. So there's a shift in terms of our accuracy," Scott MacRae, MD, said during Refractive Surgery Subspecialty Day preceding the American Academy of Ophthalmology meeting.
The current limits of myopic treatment are 10 D to 12 D of myopia, depending on corneal thickness, age and pupil size.
Current limits of hyperopic treatment are 4 D to 6 D of hyperopia. These cases are more likely than myopia cases to regress, he said.
In high levels of hyperopia, especially in patients older than 15 years, a surgeon can consider doing a clear lens extraction, Dr. MacRae said.
How Long Will My LASIK Last?
June 29, 2009
A common questin asked by my patients is "How long will my LASIK last?" The short answer is: forever for most people. This doesn't mean that you will always be 20/20. People's prescriptions change somewhat throughout life but most people will find reduced or no dependence on their glasses for many years after LASIK. A recent study published in Refractive Surgery bears this out. The authors tracked down a group of patients 14 years after laser vision correction. The majority of patients were still satisfied with their vision and their decision to have corrective eye surgery. I would expect with today's improved technology that if the same survey were conducted 14 years after LASIK performed now, the positive responses would be even higher.
Eye Specialists of Carolina
We have recently updated and expanded our practice website. For information on cataracts, intacts, refractive surgery or other services offered by Dr. Dean Dornic go to www.eyespecialistsofcarolina.com
More Information
For more information on the safety and efficacy of LASIK visit the FDA website.New and Unique Procedures
We offer a number of new and unique procedures that are unavailable at most eye centers in the country. This includes procedures for Keratoconus
Intacs
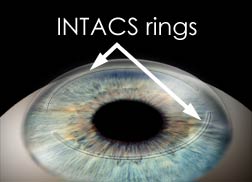 INTACS are plastic rings inserted into the mid-layer of the cornea to flatten it, changing the shape and location of the cone. INTACS may be needed when the distorted vision from keratoconus can no longer be corrected with contact lenses or eyeglasses. Intacs inserts remodel and reinforce your cornea, eliminating some or all of the irregularities caused by keratoconus in order to provide you with improved vision. The implants are removable and exchangeable. The placement of Follow-up visits will be required to monitor the healing process and evaluate the visual benefits of the procedure. Even after a successful procedure, glasses or contacts still may be required to provide you with good vision. Dr. Dean Dornic is one of the most experienced Intacs surgeons in the mid-Atlantic region. To find out if you are a candidate for Intacs arrange asurgical consultation. For more information on Intacs for the treatment of keratoconus, visit www.intacsforkeratoconus.com
INTACS are plastic rings inserted into the mid-layer of the cornea to flatten it, changing the shape and location of the cone. INTACS may be needed when the distorted vision from keratoconus can no longer be corrected with contact lenses or eyeglasses. Intacs inserts remodel and reinforce your cornea, eliminating some or all of the irregularities caused by keratoconus in order to provide you with improved vision. The implants are removable and exchangeable. The placement of Follow-up visits will be required to monitor the healing process and evaluate the visual benefits of the procedure. Even after a successful procedure, glasses or contacts still may be required to provide you with good vision. Dr. Dean Dornic is one of the most experienced Intacs surgeons in the mid-Atlantic region. To find out if you are a candidate for Intacs arrange asurgical consultation. For more information on Intacs for the treatment of keratoconus, visit www.intacsforkeratoconus.com
Collagen cross-linking is a relatively new method for treating keratoconus. It works by strengthening the corneal tissue to stop it from bulging. In this procedure, eye drops containing riboflavin (vitamin B2) are applied to the cornea and then activated by ultraviolet light. This strengthens the collagen fibers within the cornea. Corneal collagen cross-linking can reverse some of the corneal steepening and astigmatism caused by keratoconus. Numerous studies have validated the value of corneal collagen cross-linking in keratoconus. In some cases, corneal collagen cross-linking can postpone or negate the need for a corneal transplant.
Laser Corneal Transplant Surgery
Corneal Transplant Surgery is needed for patients with advanced keratoconus, where other therapies no longer provide clear vision. This usually occurs in 15-20% of cases. In corneal transplant surgery, most of the cornea is removed and then replaced with a new donor cornea. The results of the procedure have a success rate of over 97%.
Comment
There is no such thing as a medical procedure that is 100% guaranteed. Individual risk vary so please discuss your chance of success with your LASIK surgeon before proceeding.
Contact us today!
Dr. Dean Dornic
3701 NW Cary Parkway
Suite 101
Cary, NC 27513
ph: (919) 467-9955
fax: (919) 467-2544
drdeando